CHRONIC PAIN Part 1: I’m regularly in pain – but my GP just says “You’re getting old – there’s nothing to fix that” or “you’re on the highest dose of medication your body can handle’
It’s a common experience amongst some of my older patients – and a regular story I get from new patients.
If there isn’t a widely accepted treatment that their GP can write a prescription for, they get ‘sorry – can’t help’ or ‘stick with the paracetamol’ or ‘next is surgery’.
This IS more than just “there isn’t an evidence-based medication” – it’s about the time it takes for new knowledge to be translated into accepted practice in human systems.
Whether it’s the idea that doctors should wash their hands regularly (which got a lot of resistance in the 1840s); or the recognition of the role of diet in providing food for the beneficial bacteria in our bowels; or the fact that we even have beneficial bacteria all over and inside our body at all. At least 20 years will pass before general acceptance of useful ideas will manifest.
Ageing isn’t treatable – but a lot of its aches and pains can be reduced
The backbone of Naturopathic approaches are ‘evidence based’ – since time immemorial:
Lifestyle factors play a huge role.
What you eat makes a difference to the level of pain and inflammation in your body, so reduce refined processed foods and increase whole un-tampered foods. Increase things like veggies, whole grains, fruits, water, herbs and spices, eggs, fish, organic dairy and lean unprocessed meats. A Mediterranean style diet is a good start. But we are all different and have different needs and preferences.
Manage your stress levels as they effect how you perceive pain. Rewiring our brain and body nerve connections by increasing the relaxation response allows a remodelling process to occur. This is referred to as ‘neuroplasticity’.
Approaches like Massage, Cognitive Behavioural Therapy, Emotional Freedom Technique, Acupuncture – along with Herbal Medicines and supplements – can help achieve this.
Supplements with clinical evidence to back their effectiveness:
These include PEA, Curcumin, alpha-lipoic acid, magnesium, fish oils, glutamine, St Mary’s Thistle, Valerian, Corydalis, California poppy, White willow bark, Boswellia, Celery seed, Gotu cola, Lavender etc.
Herbal medicines or supplements are prescribed according to many indications, for instance the area of the body where pain is experienced or the influencers of pain like stress or fatigue level.



To assure efficacy you need to get the dose right for you as well as a reliable quality product. The right dose will depend on may things like your overall health, blood test results, family medical history, eating regime and medications consumed as well as your stage of life, cultural background and body size.
One example here is for PEA (palmitoylethanolamide):
PEA supplementation reduced pain intensity scores in patients with chronic pain
Acting as the body’s internal protective mechanism, adequate levels of palmitoylethanolamide (PEA) are required for effective management of pain and inflammation. Synthesized within the body from palmitic acid, this master molecule is a naturally occurring fatty acid mediator found in many tissues, including the brain, spinal cord, muscle, skin, blood, liver, and gastrointestinal system. Small amounts of PEA are also naturally present in a variety of plant and animal food sources.
With powerful anti-inflammatory, analgesic, antimicrobial, immuno-modulatory, and neuroprotective properties, PEA is gaining popularity for its role in reducing pain, decreasing inflammation, and supporting overall health.
For full article see Share
Anti-inflammatory and Analgesic Actions of PEA
In response to potential or actual cellular stress, whether from injury, inflammation or pain, production of PEA within local tissues increases to stop the progress of inflammation, counteract potential damage, and support the body in restoring balance.
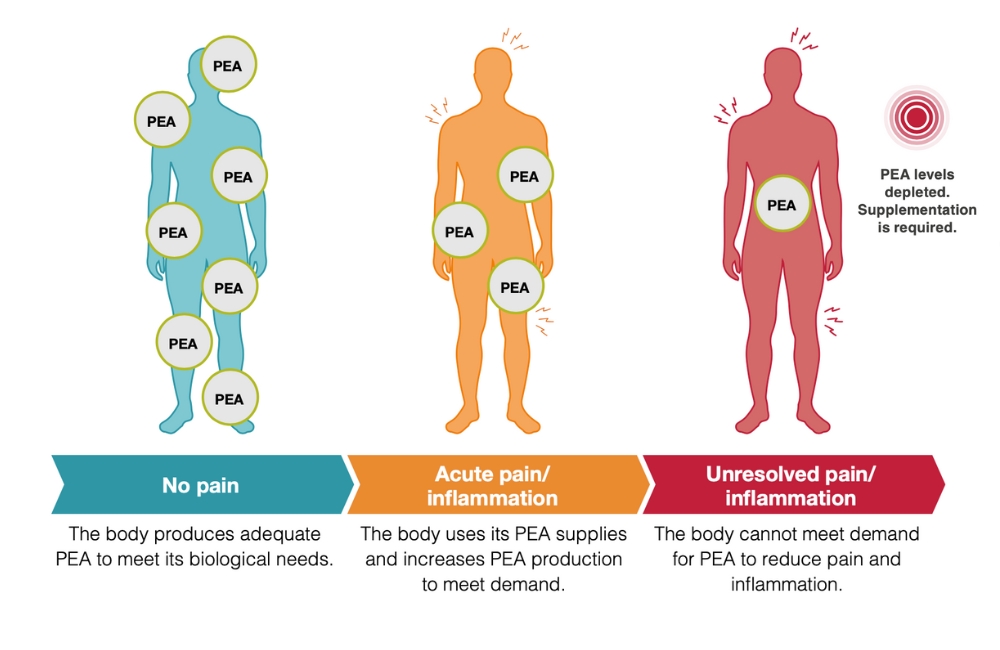
Why Chronic Pain Sufferers Need to Top Up Their PEA
In the absence of inflammation, appropriate levels of PEA can be obtained through a balanced diet and the body’s own ‘on demand’ production. However, this combination is often not enough to tackle long-lasting stress on the body, as seen in chronic inflammatory disorders, as levels can become depleted and supplementation may be required to meet the body’s needs.
There is an inverse relationship at play, with chronic inflammation hindering PEA levels, and low PEA levels impeding resolution of inflammation. (See Figure. 1)
When PEA demand outweighs supply, supplementation may be needed.
Figure. 1
Increasing research is supporting the effectiveness of PEA in pain management, with a recent 2023 systematic review and meta-analysis reporting that PEA supplementation reduced pain intensity scores, increased quality of life and improved functional status in patients with chronic pain.
PEA Supplementation Alongside Pharmaceuticals
PEA has an excellent safety profile and is generally well tolerated, non-addictive and devoid of side effects. Also, as PEA metabolism is independent from kidney and liver functions, individuals with renal and hepatic impairment can also safely supplement with PEA.
Importantly, PEA supplementation has no known drug interactions or contraindications. In fact, it can be an effective complement to pharmaceutical analgesics for the management of pain. For instance, in patients using NSAIDs to treat migraines, add-on supplementation of 1200mg/day of PEA alongside NSAIDs resulted in a statistically significant reduction in pain, and it reduced the number of attacks per month. Studies have also reported benefits to using PEA as an add-on therapy alongside opioids, with the potential for PEA to reduce opioid dose requirements, dependence and undesirable side effects. For example, PEA supplementation has been shown to delay the development of tolerance to the analgesic effects of morphine. Additionally, combination treatment of PEA and tapentadol for chronic low back pain reported significantly higher reduction in pain intensity to treatment with tapentadol alone. For references see full article above.
Absorption and Bioavailability of Supplemental PEA
Typically, standard supplemental PEA is poorly absorbed with low bioavailability, due to its poor water solubility. To counteract these absorption challenges, various advanced absorption technologies can be used. These range from reducing the particle size (micronized or ultramicronized) or making the PEA (lipid soluble) particles more water soluble.
Other help – ESSENTIAL OILS
More chronic pain relief right under our noses: Essential oils from plants may provide an easy to apply solution for many people. Usually applied externally (and mostly diluted with other oils – seek guidance) these oils can influence different types of pain for the better.
Your olfactory nerves (nerves in your nose to brain connection) influence how your brain reacts to pain. You may find Lavender soothing for your headache or Peppermint with Chamomile oil may calm your digestive pain even by just sniffing it. Eucalyptus or Marjoram essential oil can be wonderful for aching joints and muscular pain.
Find trusted sources of information to help you understand applications and benefits and address safety issues with these concentrated potentially toxic molecules. Caution: some people are highly sensitive and reactive to essential oils.
See Part 2 coming up for more help with chronic pain
Confer with your experienced informed Naturopath for further information and a Consultation to best help you.